Pericardial Effusion
Jump to content
Definition Aetiology Pathophysiology Risk factor Sign and Symptoms Investigations Management
Definition
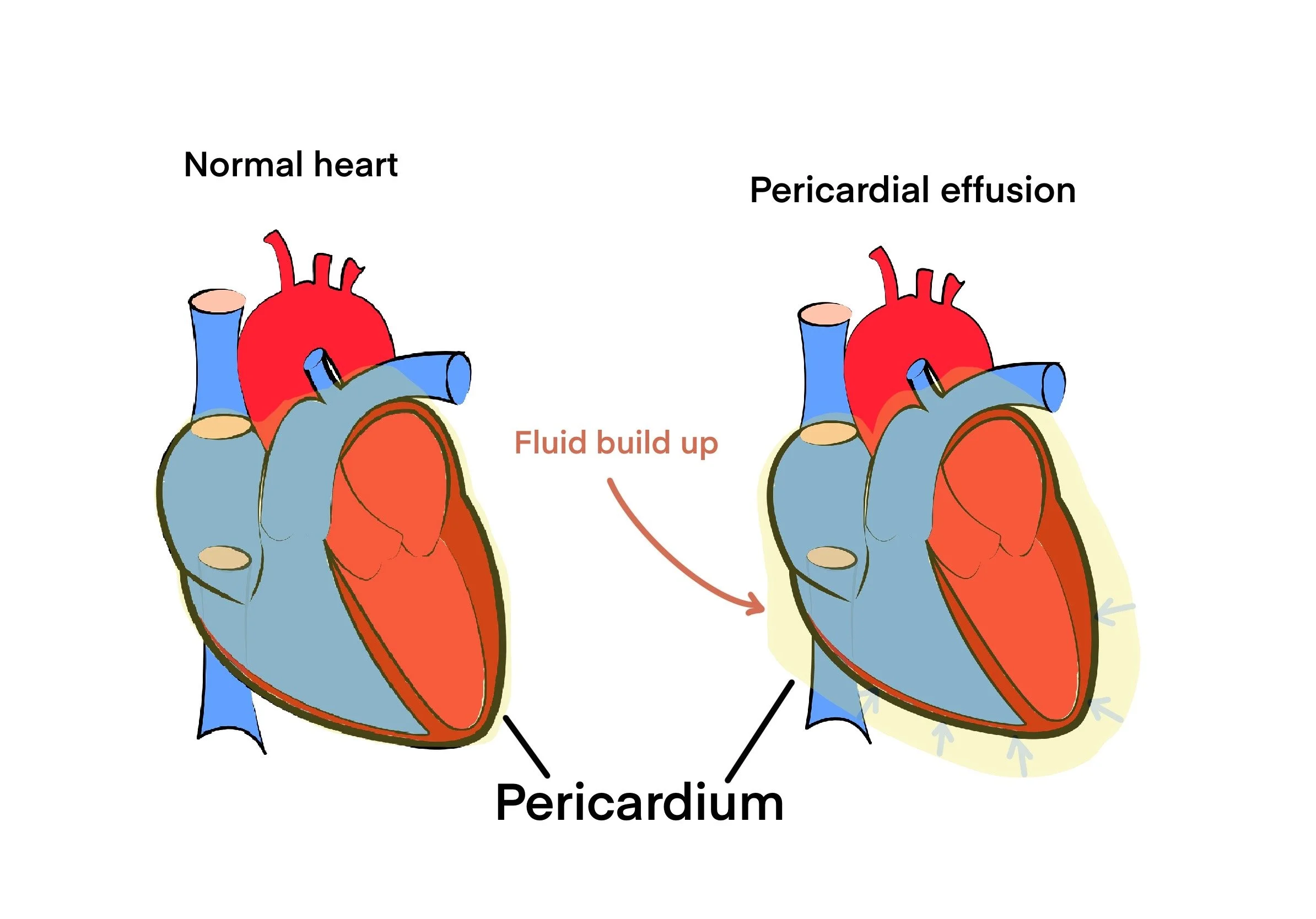
Pericardial effusion is the medical term used to define the accumulation of fluid in the pericardial cavity. This is the area or space surrounding the heart (see figure 1). This event could lead to an increase in heart’s pressure, which could cause chest pain, shortness of breath, and low blood pressure.
Figure 1
Fluid build up can be seen on Right illustration of the heart.
Aetiology
Infections: Viral or bacterial infections can cause swelling of the pericardium, which causes fluid build up. Coxsackie B and adenovirus infections are the most typical causes.
Inflammatory causes: Rheumatoid arthritis, lupus, and other autoimmune conditions can cause the pericardium to become inflamed, which can result in pericardial effusion.
Cancer: Pericardial effusion can result from lung, breast, and stomach tumours that have spread to the pericardium.
Trauma: A chest trauma may cause bleeding into the pericardial cavity, which could result in pericardial effusion.
Idiopathic: no known cause.
Pathophysiology
A typical fluid that can build up in the pericardial space is blood. As a result, there is a decrease in cardiac output and interference with the heart's capacity to fill its chambers. Extreme cases of fluid accumulation can result in a cardiac tamponade, a potentially fatal condition in which the heart's pressure rises to a point where it cannot adequately supply the body with blood, leading to organ failure and, if left untreated, it can lead to death.
Risk factors
Pericarditis: Individuals with a history of previous pericarditis (inflammation of the pericardium)
Cancer
Heart failure
Autoimmune diseases: Rheumatoid arthritis (RA) and lupus
Medications: for example hydralazine and procainamide,
Radiation therapy: radiation therapy performed around the chest area are at risk for pericardial effusion
Idiopathic
Trauma
Sign and symptoms
Chest pain
Shortness of breath (SOB) caused by buildup of fluid in the pericardial cavity.
Hypotension: caused by reduced cardiac out due to increased pressure on the heart.
Tachycardia
Fatigue
Peripheral edema.
Cough
In severe cases, cardiac tamponade
Investigations
Blood tests: FBC, CRP, ESR to check for the presence of raised inflammatory markers which could be linked to pericardial effusion.
Echocardiography
Computed Tomography (CT) scan
Magnetic Resonance Imaging (MRI)
Pericardiocentesis: a needle is inserted into the pericardial cavity to drain the fluid.
Biopsy
Cardiac catheterization: normally used to check the pressure in the pericardial cavity.
Management
Pericardiocentesis
Treat underlying cause: infection? Inflammation? Autoimmune?
Surgery: repair/removal of pericardium or removal of tumour (if cancer present)
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.