Paroxysmal Supraventricular Tachycardia (PSVT)
Definition | Aetiology | Pathophysiology | Risk Factors | Signs and Symptoms | Investigations | Diagnosis | Management
Definition
Paroxysmal supraventricular tachycardia (PSVT) is a condition characterized by a rapid heart rate that originates above the ventricles (the lower chambers of the heart). The term "paroxysmal" refers to the episodic nature of this condition, with episodes occurring either frequently or infrequently, sometimes years apart. In PSVT, the heart rate is regular, rapid, and can start and stop suddenly.
Aetiology
PSVT can develop due to a variety of medical conditions and medications, including:
- Hyperthyroidism
- Alcohol
- Chronic Lung Disease: Asthma, COPD
- Chest Wall Trauma
- Digoxin Toxicity
- Pericarditis
- Hypoxia
- Mitral Valve Prolapse
- Cardiomyopathy
- Pneumonia
- Myocarditis
- Hypovolemia
- Anxiety
- Salbutamol
- Cocaine
- Myocardial Infarction (MI)
- Pulmonary Embolism (PE)
- Verapamil
- Structural Heart Disease
- Caffeinated Beverages
Pathophysiology
PSVT is primarily caused by a short circuit or an abnormal electrical pathway in the heart, leading to rapid heartbeats. The three main types of PSVT include:
- Atrioventricular Nodal Re-entrant Tachycardia (AVNRT):
This occurs when there is an extra signalling pathway in or near the atrioventricular (AV) node. This extra pathway rapidly sends electrical impulses, causing sudden and fast heartbeats.
- Wolff-Parkinson-White Syndrome (WPW):
WPW involves additional muscle fibres connecting the atria and ventricles, forming an accessory electrical pathway that creates a loop circuit. This congenital disorder can lead to severe tachycardia, and catheter ablation may be required for a cure.
- Atrial Tachycardia:
This occurs when an electrical impulse in the atria originates from an unexpected location and rapidly repeats, causing tachycardia.
Risk Factors
Several factors increase the likelihood of developing PSVT:
- Gender: Women are twice as likely to develop PSVT.
- Pneumonia
- Current Alcohol Intoxication
- Heart Diseases
- Asthma Medications: Certain medications used to treat asthma can trigger PSVT.
- Previous Myocardial Infarction
- Digoxin Toxicity
- Previous Heart Surgery
- Age: The risk increases with age, particularly after 65 years.
- Obesity
- Chronic Lung Disease: Asthma, COPD
- High Caffeine Intake
- Illicit Drugs: Usage can increase the risk of PSVT.
- Smoking
Signs and Symptoms
Common symptoms of PSVT include:
- Palpitations: Sensation of a rapid, fluttering, or pounding heart.
- Light-Headedness
- Weakness
- Fatigue
- Shortness of Breath (SOB)
- Chest Pressure
- Syncope: Fainting or near-fainting episodes.
Investigations
Diagnostic investigations for PSVT include:
- 12-Lead ECG: The primary tool for diagnosing PSVT, showing a regular but narrow complex tachycardia (see Image 1).
- 24-Hour ECG: Continuous ECG monitoring to capture intermittent episodes.
- Troponin Blood Test: To assess for myocardial infarction if the patient presents with chest pain symptoms.
- Blood Tests: Full blood count (FBC), urea and electrolytes (U&E), thyroid function tests (TFT).
- Chest X-ray (CXR): To rule out other causes, such as pneumonia or heart failure.
- Echocardiogram: To assess heart structure and function.
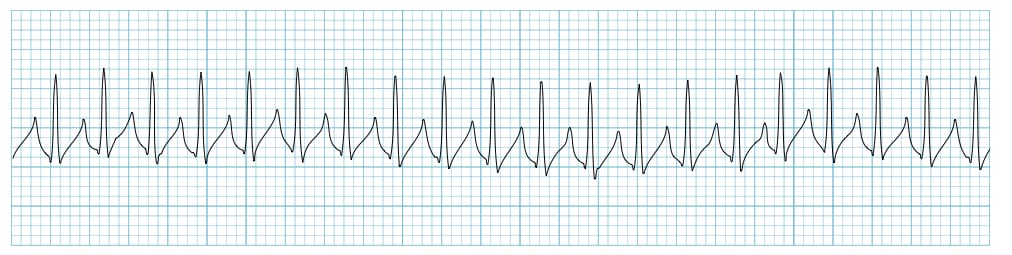
Image 1: This ECG demonstrates a regular but narrow complex tachycardia, characteristic of supraventricular tachycardia (SVT). Note the rapid heart rate with a consistent rhythm, indicating the presence of PSVT.
Diagnosis
PSVT is typically diagnosed based on physical examination and ECG findings:
- Physical Examination: May reveal dizziness, palpitations, and tachycardia.
- ECG: Confirmatory diagnosis through the presence of regular, narrow complex tachycardia.
Management
Management of PSVT focuses on controlling heart rate and addressing the underlying cause:
- If Acutely Unwell: The patient should be admitted to the hospital for urgent management.
- Vagal Manoeuvres: Techniques such as the Valsalva manoeuvre or carotid sinus massage can be used to activate the vagus nerve and slow down the heart's electrical impulses.
- Medication: If vagal manoeuvres fail, adenosine is the first-line treatment, followed by verapamil if needed.
- Electrical Cardioversion: Used in emergency situations where medications are ineffective. This involves delivering controlled electrical impulses to restore normal rhythm, typically under general anaesthesia.
- Catheter Ablation: A definitive treatment option for recurrent PSVT, involving the removal or modification of the abnormal tissue causing the arrhythmia.
References
- Life in the Fast Lane (LITFL) (2018) Supraventricular Tachycardia (SVT) Rhythm Strip. Available at: https://litfl.com/wp-content/uploads/2018/08/Supraventricular-tachycardia-SVT-Rhythm-Strip.jpg (Accessed: 26 August 2024).
- British Heart Foundation (2024) Understanding Supraventricular Tachycardia. Available at: https://www.bhf.org.uk (Accessed: 26 August 2024).
Previous Topic (Atrial Fibrillation)
Next Topic (Ventricular Fibrillation)
Check out our youtube channel
Blueprint Page
Explore the comprehensive blueprint for Physician Associates, covering all essential topics and resources.
Book Your Session
Enhance your skills with personalised tutoring sessions tailored for Physician Associates.

